1. Initial investigation and referral
The first point of medical contact may be your general practitioner (GP) or a doctor in an emergency department. The doctor will assess your symptoms (for example, a lump or a painful swelling), conduct a physical examination and arrange tests.
Tests you may have:
- Blood tests: To check your overall health, how your blood cells, liver and kidneys are working.
- Magnetic resonance imaging (MRI) scan: Magnetic fields and radio waves are used to take pictures of the inside the body.
- Computed tomography (CT) scan: Computer technology and x-rays are used to create detailed images of the body.
Your GP should also discuss your needs (including physical, psychological, social and information needs) and recommend sources of reliable information and support.
If sarcoma is suspected, you must be referred promptly to a sarcoma specialist for further testing. Your GP will provide the specialist with information about your medical history, whether there is a history of cancer in your family, and results of the initial tests.
It can be helpful to bring a family member or friend with you to your appointments.
2. Diagnosis and staging
Your specialist will discuss your test results with you and what further tests are required. Your specialist will send you to get tests to check whether cancer is present and, if it is, its stage of development. Your specialist should arrange a biopsy. These test should be done within 2 weeks.
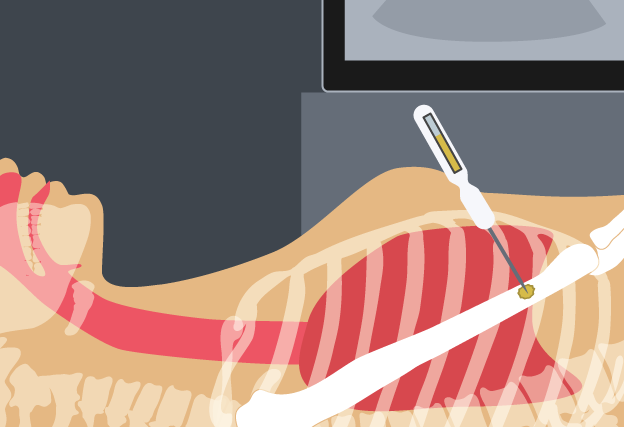
CT guided biopsy
This is the most common method of biopsy for a soft tissue or bone tumour. A sample of cells will be taken from the lump using a needle with local anaesthetic to numb the area. CT scan is used to guide the biopsy needle. Biopsies for bone and soft tissue cancers are specialised procedures and should only be carried out by a specialist who does them regularly. An expert pathologist will then look at the sample of cells under a microscope and determine the exact diagnosis. This may involve special testing of the cells and usually takes several days, sometimes longer.
It can be helpful to contact peer support groups, and support groups for carers.
3. Treatment
The term sarcoma describes over fifty different types of cancer, each of which may be treated differently. To ensure you receive the best care, your specialist will arrange for a team of health professionals to plan your treatment based on your preferences and needs. Your specialist will tell you when the team will be discussing your case.
Your team will plan your ongoing care, and should discuss the different treatment options with you including the likely outcomes, possible side effects and the risks and benefits.
Let your team know about any complementary therapies you are using or thinking about trying. Some therapies may not be appropriate, depending on your medical treatment.
If appropriate, your team should also discuss the option of fertility preservation and having a baby in the future. You may be referred to a fertility service to help you evaluate your options.
Treatment options:
Treatment for bone sarcoma and soft tissue sarcoma may include surgery, chemotherapy and radiotherapy in a range of combinations.
Surgery
Surgery is the most common treatment for most types of sarcoma. The type of surgery used will depend on where the cancer is and its size. It is important that this surgery is performed by a surgeon who is very experienced in surgery on sarcoma and performs several of these operations every year.

Reconstructive surgery
Reconstructive surgery aims to restore function and appearance to the affected area after surgical removal of bone or tissue. When this involves the limb, the preference is for reconstruction (limb salvage surgery). Reconstruction can involve replacing bone, soft tissue, or function of muscles and nerves.

Limb ablative surgery (amputation)
Occasionally it is not possible to remove all of the cancer without badly affecting the arm or leg. The doctor may advise that the only effective treatment will be to remove the limb.

Radiation therapy
Radiation therapy (also called radiotherapy) may be given to you before or after surgery and is most often used for soft tissue sarcomas.

Chemotherapy
Chemotherapy may be given to you either before surgery to try and shrink the cancer, or after surgery to stop it coming back. It is most often used for bone sarcomas.

Your doctor may also suggest you consider taking part in a clinical trial using newer or experimental therapies.
For more information about treatment and treatment side effects ask your doctor or visit our treatment section.
Your specialist should discuss your needs with you during and after treatment (including physical, psychological, social and information needs) and may refer you to another service or health professional for different aspects of your care.
4. After treatment
During treatment, a rehabilitation program may be developed for you. If you had an amputation, this will include seeing a specialist who makes false (prosthetic) limbs. A physiotherapist or exercise physiologist can help you become as independent and mobile as possible.
After treatment is completed, your specialist team will see you regularly for follow-up appointments. During these visits your specialist will arrange tests to watch for signs of cancer recurrence or treatment side effects and support your return to health.
Your doctor should provide you with a treatment summary that details the care you received, including:
- diagnostic tests performed and their results
- types of treatment used and when they were performed
- treatment plans from other health professionals
- supportive care services provided to you
- contact information for key care providers.
You and your GP will receive a follow-up care plan that tells you:
- the type of follow-up that is best for you
- ways to manage any side effects of treatment, should they occur
- how to get specialist medical help quickly if you think the cancer has returned or got worse.
Your doctor should:
discuss your needs with you and refer you to appropriate health professionals and/or community organisations, if support is required
provide information on the signs and symptoms to look out for that might mean a return of the cancer
provide information on prevention and healthy living
Sarcoma can come back after treatment. This is why it is important that you have regular check-ups.
5. Living with cancer
Side effects:
Some people experience side effects (for example, tiredness) that continue beyond the end of treatment. Sometimes side effects don’t begin until months after treatment has finished. For more information about side effects ask your doctor.
Advance care plan:
Your doctor may discuss with you the option of developing an advance care plan. An advance care plan is a formal way of setting out your wishes for future medical care. For more information about advance care planning ask your doctor or visit advancecareplanning.org.au.
Palliative care:
This type of treatment could be used at different stages to help you with pain relief, to reduce your symptoms or help improve your quality of life. For more information about palliative care ask your doctor or visit palliativecare.org.au.
6. Questions of cost
There can be cost implications at each stage of the cancer care pathway, including costs of treatment, accommodation and travel. There can be substantial out-of-pocket costs if you are having treatment in a private health service, even if you have private health insurance.
You can discuss these costs with your doctor and/or private health insurer for each type of treatment you may have. If you are experiencing financial difficulties due to your cancer treatment you can contact the social worker at your local hospital.
For more information visit costs of treatment.
For more information about accommodation and travel costs visit our support section.
7. Further support
Sarcoma cancer support
For information about bone or soft tissue sarcomas or where to go for support call Cancer Council on 13 11 20. Specially trained staff can answer your questions about the effects of cancer, explain what will happen during treatment or link you to support groups and other community resources.
If you need an interpreter, call TIS (the Translating and Interpreting Service) on 1314 50.
For support and advice for carers, call the Carers Association on 1800 242 636.
More support options
Australian Cancer Survivorship Centre
Has general and tumour-specific information, primarily focused on the post-treatment survivorship phase
• Telephone: (03) 9656 5207
• Website: www.petermac.org/cancersurvivorship
National Health Services Directory
A directory providing information on local hospital and community services
• Website: www.nhsd.com.au
beyondblue: the national depression initiative
Information on depression, anxiety and related disorders, available treatment and support services
• Telephone: 1300 22 4636
• Website: www.beyondblue.org.au
Cancer Australia
Information on cancer prevention, screening, diagnosis, treatment and supportive care for Australians affected by cancer, and their families and carers
• Telephone: 1800 624 973
• Website: www.canceraustralia.gov.au
Care Search: Palliative Care Knowledge network
Information for patients and carers on living with illness, practical advice on how to care, and finding services
• Telephone: (08) 7221 8233
• Website: www.caresearch.com.au
Optimal care pathways have been developed for health professionals and health services. However, patients and carers may find useful information in this version to help understand the processes their treating health professionals are following.

