1. Initial investigation and referral
Your general practitioner (GP) will assess your symptoms (such as persistent pain, weight loss, a lump), conduct a thorough physical examination and arrange blood tests. Your GP may also order other tests (for example, urine and faecal tests, x-ray), depending on your symptoms. Your GP should also discuss your needs (including physical, psychological, social and information needs) and recommend sources of reliable information and support.
If cancer is suspected, you will be referred to a specialist for further testing. The specialist appointment should be done within 2 weeks of the initial referral. The specialist you see first will depend on the symptoms you have. Your GP will provide the specialist with information about your medical history, whether there is a history of cancer in your family, and your test results.
It can be helpful to bring a family member or friend with you to your appointments.
2. Diagnosis and staging
Your specialist will discuss your test results with you and options for further testing. Your specialist will send you to get tests to check whether cancer is present and, if it is, its stage of development. Your specialist should arrange a biopsy if you are well enough and if you haven’t had one already. These test should be done within 2 weeks.
It can be helpful to contact cancer peer support groups and support groups for carers.
Biopsy
A minor surgical procedure where the doctor removes a small amount of tissue for examination under a microscope. A local or general anaesthetic may be used. This may also include genetic testing of the tumour to help in providing a 'best guess' of the location of the cancer.
Your specialist will send you to get tests to check whether cancer is present and, if it is, its stage of development.
3. Further referral and testing
Cancer of unknown primary (CUP) is when cancer cells are found in the body but the place the cancer began is not known.
If CUP is detected, to ensure you receive the best care, your specialist may need to refer you to another doctor. The doctor will be part of a team made up of professionals who have experience managing and supporting a person with CUP (if not specialising in this area themselves), or in a specialist cancer centre.
Because CUP has already spread, further tests are usually done, based on the site of the secondary cancer/s and any ‘clues’ as to where the cancer may have started from your initial tests. Tests are ordered to ensure that cancers which are still curable or treatable, even when spread, are not missed.
Your team will plan further tests and treatment based on your preferences, symptoms, and previous test results. Your specialist will tell you when the team will be discussing your case.
You may have one or more of the following tests (some of these tests are not covered by Medicare):
Tumour marker test
A sample of blood or tissue is checked to measure the amounts of certain substances made by tumour cells in the body.

Ultrasound
This uses high-frequency sound waves to make an image of a person’s internal body structures.
Positron emission tomography (PET) scan
This produces a three-dimensional image that may show where cancers are located. A small amount of radioactive material is injected, and the whole body is scanned.

Magnetic resonance imaging (MRI) scan
MRI's are when magnetic fields and radio waves are used to take pictures inside the body.
Computed tomography (CT) scan/bone scan
Computer technology and x-rays are used to create detailed images of the body.

Gastroscopy and/or colonoscopy
A long flexible tube with a camera on it (called an ‘endoscope’) is inserted via your mouth or anus under a light general anaesthetic, and the images appear on a screen.
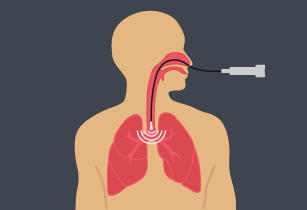
Some people have further tests such as a bronchoscopy or mammogram.
Sometimes, these tests will find the primary cancer at the time of diagnosis or sometimes it might be found later in the course of the illness. When this happens, the cancer is no longer called CUP and is treated according to the place of origin.
If your specialist can’t be sure of the primary cancer, they may be able to suggest a possible part of the body where the cancer started (based on where the secondary cancers are, your symptoms and the test results). This will help your team to plan your treatment.
4. Treatment
Your team should discuss the different treatment options with you including the likely outcomes, possible side effects and the risks and benefits. You might want to ask for more time before deciding on your treatment, or ask for a second opinion. Let your team know about any complementary therapies you are using or thinking about trying. Some therapies may not be appropriate, depending on your medical treatment.
Treatment options for CUP:
For most cancers, treatment is determined by the type of cancer and depends on correct diagnosis and staging. Because the primary cancer type is unknown, the types of treatments used for CUP are quite variable. The doctor will discuss with you a recommended approach based on all the available test results and the most likely type of primary cancer.
For most patients with CUP, current treatments do not cure the cancer. However, treatment may be able to control the cancer and improve your symptoms. In a minority of cases, CUP can be treated effectively or even cured if is contained in just one area of the body. The main treatment used for CUP is chemotherapy. Other treatments may include radiation therapy, surgery or hormone treatment, or a combination of these.
Chemotherapy
May be given to try to shrink the cancer or try and slow its growth.

Radiation therapy
(Also called radiotherapy) may be given to you in combination with chemotherapy.
Surgery
May be suitable if the cancer is found only in the lymph nodes or in one organ, or to help with symptoms.

Hormone therapy
May be suitable if your test results show that you may have a cancer that has hormone receptors (usually breast, prostate, womb, and kidney cancers).

Your doctor may also suggest you consider taking part in a clinical trial using newer or experimental therapies.
Palliative treatment:
A palliative care team may oversee your treatment, or be available to help support you, to ensure that your physical and emotional needs are being met.
5. After treatment
After your primary treatment is completed, your doctor should provide you with a treatment summary that details the care you received including:
- diagnostic tests performed and their results
- types of treatment used and when they were performed
- treatment plans from other health professionals
- support services provided to you.
Your doctor will decide whether your ongoing care will be managed by your GP, a palliative care physician, or whether you should continue to see your specialist. You will both receive a follow-up care plan that tells you about:
- the type of follow-up that is best for you
- care plans for managing any side effects of treatment
- how to get medical help quickly.
If you need extra help after treatment, your GP or palliative care physician can discuss your needs with you and refer you to appropriate health professionals and/or community organisations.
6. Living with cancer
Your doctor should discuss your needs with you during and after treatment (including your physical, psychological, social and information needs) and may refer you to another service or health professional for different aspects of your care.
Side effects:
Some people experience side effects (for example, tiredness) that continue beyond the end of treatment. Sometimes side effects don’t begin until months after treatment has finished. For more information about side effects ask your doctor.
Advance care plan:
Your doctor may discuss with you the option of developing an advance care plan. An advance care plan is a formal way of setting out your wishes for future medical care. For more information about advance care planning ask your doctor or visit advancecareplanning.org.au.
Palliative care:
This type of treatment could be used at different stages to help you with pain relief, to reduce your symptoms or help improve your quality of life. For more information about palliative care ask your doctor or visit palliativecare.org.au.
7. Questions of cost
There can be cost implications at each stage of the cancer care pathway, including costs of treatment, accommodation and travel. There can be substantial out-of-pocket costs if you are having treatment in a private health service, even if you have private health insurance.
You can discuss these costs with your doctor and/or private health insurer for each type of treatment you may have. If you are experiencing financial difficulties due to your cancer treatment you can contact the social worker at your local hospital.
For more information visit costs of treatment.
For more information about accommodation and travel costs visit our support section.
8. Further support
Cancer of unknown primary (CUP) support
For information about CUP or where to go for support call Cancer Council on 13 11 20. Specially trained staff can answer your questions about the effects of cancer, explain what will happen during treatment or link you to support groups and other community resources.
If you need an interpreter, call TIS (the Translating and Interpreting Service) on 13 14 50.
For support and advice for carers, call the Carers Association on 1800 242 636.
More support options
Australian Cancer Survivorship Centre
Has general and tumour-specific information, primarily focused on the post-treatment survivorship phase
• Telephone: (03) 9656 5207
• Website: www.petermac.org/cancersurvivorship
beyondblue: the national depression initiative
Information on depression, anxiety and related disorders, available treatment and support services
• Telephone: 1300 22 4636
• Website: www.beyondblue.org.au
Cancer Australia
Information on cancer prevention, screening, diagnosis, treatment and supportive care for Australians affected by cancer, and their families and carers
• Telephone: 1800 624 973
• Website: www.canceraustralia.gov.au
Care Search: Palliative Care Knowledge network
Information for patients and carers on living with illness, practical advice on how to care, and finding services
• Telephone: (08) 7221 8233
• Website: www.caresearch.com.au
Optimal care pathways have been developed for health professionals and health services. However, patients and carers may find useful information in this version to help understand the processes their treating health professionals are following.